Total Knee Replacement Postoperative Patient Instructions
Post-op Office Visit: Please note that your 1st post-op visit has been scheduled for 2-3 weeks after your surgery. If you do not already have or know your appointment date and time, please contact our office as soon as possible at 713-441-3569.
Activities: Unless otherwise instructed, you are encouraged to bear as much weight as possible when walking. A walker should be used until you are able to use a cane. If you feel you are able to do so, you may transition use from a walker to a cane. A cane is used in the OPPOSITE hand of your operative leg. You should be walking every 2 hours during the day. Start with short distances and progress to longer distances as you are able.
Home Health: Upon insurance approval, you will begin receiving home health visits, which is arranged by our office or by the social worker/case manager from the hospital prior to your discharge. Please know that patients with Medicare coverage are only accepted by the home health agency with which we have a contract. Should you not receive home health visits, you can work on the exercises shown on this sheet until you start outpatient physical therapy.
Physical Therapy: We highly recommend at least 4-6 weeks of outpatient therapy for ALL patients who have undergone knee replacement surgery. This will ensure that you regain range of motion and strength after surgery. Please note that it is YOUR responsibility to schedule your therapy. Therapy should begin no later than one week after your surgery. An order for physical therapy will be provided in your chart. Should you wish to go to a Houston Methodist physical therapy facility, they will have access to this order and can schedule therapy sessions with you. If you decide to go elsewhere for therapy, they will require a faxed order for therapy before scheduling or at least before the first visit. Please provide our office with their fax number so that we can send the order in a timely manner.
Incision Care: Do not remove your surgical dressing unless advised to do so by Dr. Incavo or his staff. Your surgical dressing is impregnated with silver (an antibiotic), which allows the dressing to stay on until your first post-operative office visit. This dressing is waterproof, therefore YOU MAY SHOWER after your surgery with the dressing intact. If the dressing becomes loose around the edges, you may reinforce it with tape. It is normal for some drainage to appear in the dressing—it does not require to be changed unless it is fully saturated or starts to leak out the side.
It is not unusual to have pain, swelling, redness, bruising, warmth, and/or numbness in the areas surrounding the surgical site following surgery. Pain or bruising of the thigh region is likely due to the temporary tourniquet placed on your thigh during surgery to minimize blood loss. To address your pain and swelling, it is important that you take time to rest and elevate the operative leg above the level of the heart. You may also place ice over the surgical area twenty minutes at a time. Should you develop significant swelling and tenderness of the calf that does not respond to this treatment, please contact our office or submit a message via MyChart.
Anticoagulants: You will require a blood thinning medication after surgery to decrease the risk of blood clots. Most patients will be instructed to take Aspirin 81 mg (baby aspirin) twice daily for 4 weeks. However, if you have a history of blood clots or embolism, you may likely be placed on another form of anticoagulation. Patients already on a prescription blood thinner like Coumadin, Plavix, Xarelto, or Eliquis will be instructed to restart these medications on a day indicated by Dr. Incavo or his staff.
Pain Medications: You will be discharged from the hospital with prescription(s) for pain medication. Take the pain medication as prescribed and only for as long as you have pain. The pain medications are only to be taken as needed. For the first few days, you may likely require dosing more often (ie. Every 6 hours), but you may reduce the frequency of use as you can tolerate. You should NOT OVERUSE these medications due to side effects, which may include: nausea, itching, constipation, drowsiness as well as dependence. Prescriptions for narcotic medications will generally NOT BE written for longer than 6 weeks after your surgery and cannot be called into your pharmacy. PLEASE NOTE DUE TO DEA REGULATIONS, ALL NARCOTIC PRESCRIPTIONS WILL HAVE TO BE HANDWRITTEN ON A TRIPLICATE PRESCRIPTION AND WILL ONLY BE AVAILABLE TO BE PICKED UP IN THE OFFICE DURING NORMAL BUSINESS HOURS.
Constipation: Constipation can easily occur when patients are hospitalized, given general anesthesia and given large doses of pain medications. You should increase your fiber, fluids and bowel regulating foods to your diet prior to surgery. Good foods include prunes, prune juice, whole grain breads, oatmeal, fruits and vegetables. Fiber supplements such as Metamucil, Citrucel, or FiberCon can also be helpful. If you are unable to have a bowel movement by the third day following surgery a laxative may be necessary. There are many good over the-counter medications that you may use including: Colace, Sennakot, Phillips Milk of Magnesia, Miralax, Dulcolax. If you are still unable to achieve a bowel movement with these methods, a glycerin suppository or use of an enema may be necessary.
Driving: You may return to driving 2 weeks after surgery once you are walking comfortably with a cane.
Dental Visits: Dental procedures should be postponed for 6 months after joint replacement surgery. When you do return to the dentist, antibiotics will need to be taken 1 hour prior to your visit to prevent infection of the joint replacement. Please inform your dentist that you have a joint replacement. Antibiotics can be prescribed by our office or by your dentist. You will take Amoxicillin 2000 mg (four 500 mg tablets) 1 hour prior to dental work. If you are allergic to penicillin, you will be given Clindamycin 900 mg (three 300 mg tablets) to be taken 1 hour prior to procedure. If a dental visit is necessary or urgent before 6 months after joint replacement, please contact our office.
If you have any additional questions please contact our office at 713-441-3569 or via MyChart.
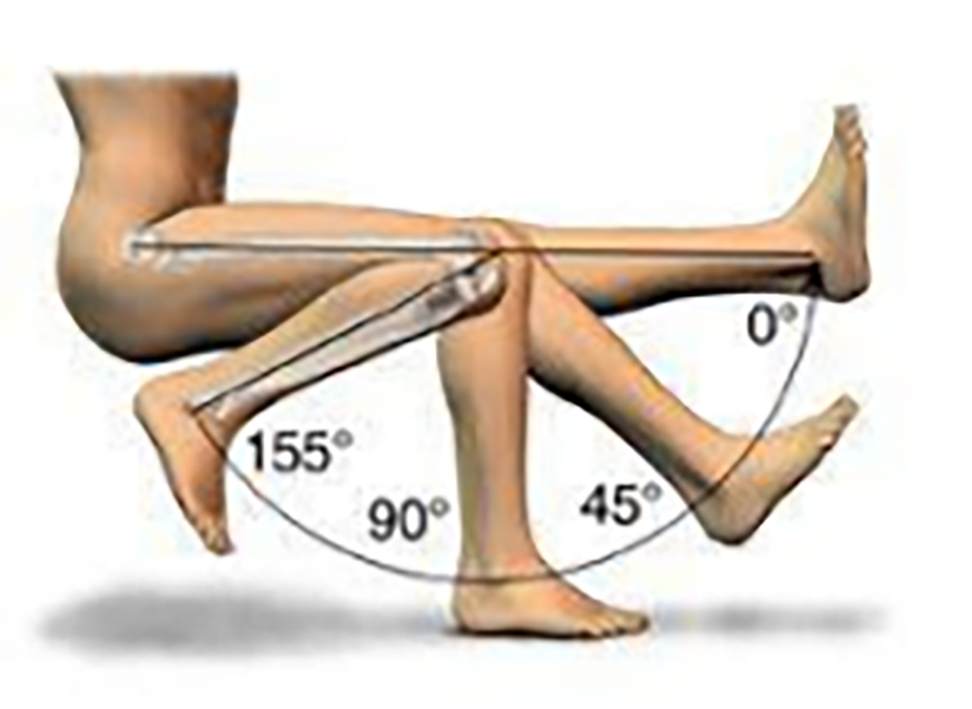
Knee Range of Motion Reference:
0 degrees is when the knee is perfectly straight.
90 degrees is when the angle between the thigh and shin is 90 degrees, like when sitting in a chair
Goal: Move the knee from 0-90 by 2 weeks, with end-goal being 0-120 degrees after 6 weeks of therapy.

Knee Extension:
Sit in a chair and place your heel on a padded chair or stool with nothing underneath the knee. You may leave the leg like this while you watch tv or read a book. Over time, the knee will straighten.
You can place gentle pressure on your thigh/knee to help straighten it. Press down for 10-20 seconds until you feel a stretch, then relax. Repeat 10 times.

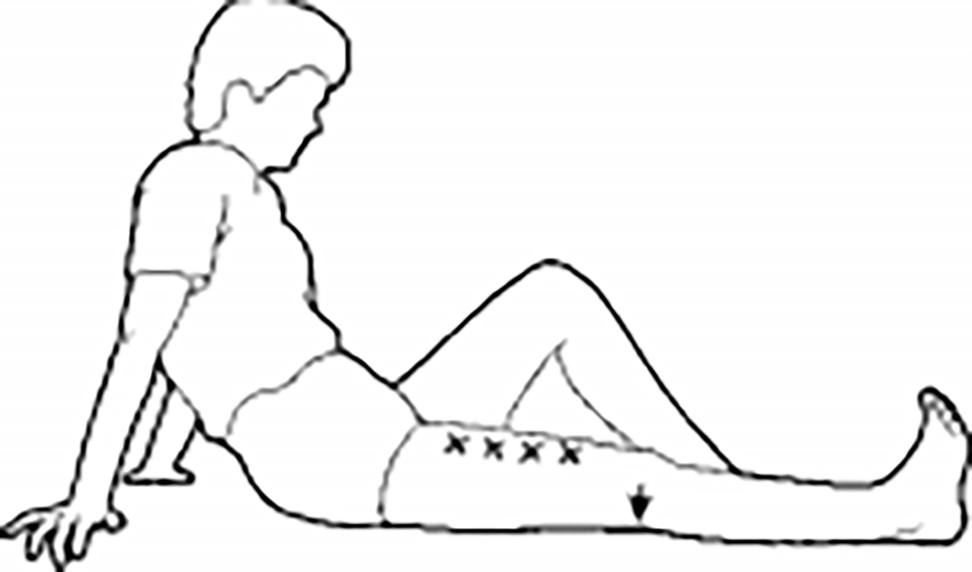
Knee Flexion:
While seated, slide your foot back along the floor so the knee
bends. Cross your non-operative leg over and use it to help
pull your operative leg back so that the knee bends. Your goal
is to have the knee bend to 90 degrees by 2 weeks.
Work on the above exercises 2-3 times daily for 10-20 minutes at a time.
Quad Sets for Quad Strengthening
Lie on your back or sit upright with your leg straight.
Push your knee into the floor by tightening your thigh
muscles.Hold for 10 seconds, relax. Repeat 10-20 times 2-3 times daily.

Straight Leg Raises
Lie on your back or sit upright with your operative leg straight. ∙ Raise your leg off the bed or above the chair and work to hold for 30 seconds.
Repeat 10-20 times. Repeat 2-3 times daily.

Ankle Pumps (To prevent blood clots)
Stand holding on to a solid object for support and balance.
Raise your heels off the floor standing on the balls of your feet.
Total Hip Replacement Postoperative Patient Instructions
Post-op Office Visit: Please note that your 1st post-op visit has been scheduled for 2-3 weeks after your surgery. If you do not already have or know your appointment date and time, please contact our office as soon as possible at 713-441-3569.
Activities: Unless otherwise instructed, you are encouraged to bear as much weight as possible when walking. A walker should be used until you are able to use a cane. If you feel you are able to do so, you may transition use from a walker to a cane. A cane is used in the OPPOSITE hand of your operative leg. You should be walking every 2 hours during the day. Start with short distances and progress to longer distances as you are able.
Hip Precautions: You will need to maintain hip precautions for the first 6 weeks after surgery. This includes not bending at the waist past 90 degrees, not crossing your legs at the knees, and avoid turning your toes inward. Avoid sitting on very low seats, sofas, and beds. Following these guidelines significantly decreases the risk of postsurgical complications like hip dislocation.
Home Health: Upon insurance approval, you will begin receiving home health visits, which is arranged by our office or by the social worker/case manager from the hospital prior to your discharge. Please know that patients with Medicare coverage are only accepted by the home health agency we utilize.
Physical Therapy: We do not recommend any formal physical therapy for patients with hip replacement surgery. Please see exercises in this packet for the recommended self-guided exercises that you can do at home. We recommend that you work on these exercises 5-10 minutes at a time twice daily. If outpatient physical therapy is recommended this will be done by Dr. Incavo at the first postoperative visit.
Incision Care: Do not remove your surgical dressing unless advised to do so by Dr. Incavo or his staff. Your surgical dressing is impregnated with silver (an antibiotic), which allows the dressing to stay on until your first post-operative office visit. This dressing is waterproof, therefore YOU MAY SHOWER after your surgery with the dressing intact. If the dressing becomes loose around the edges, you may reinforce it with tape. It is normal for some drainage to appear in the dressing—it does not require to be changed unless it is fully saturated or starts to leak out the side.
It is not unusual to have pain, swelling, redness, bruising, warmth, and/or numbness in the areas surrounding the surgical site following surgery. To address your pain and swelling, it is important that you take time to rest and elevate the operative leg above the level of the heart. You may also place ice over the surgical area twenty minutes at a time. Should you develop significant swelling and tenderness of the calf that does not respond to this treatment, please contact our office or submit a message via MyChart.
Anticoagulants: You will require a blood thinning medication after surgery to decrease the risk of blood clots. Most patients will be instructed to take Aspirin 81 mg (baby aspirin) twice daily for 4 weeks. Unless you have a history of blood clots or embolism, you will then be placed on another form of anticoagulation. Patients already on a prescription blood thinner like Coumadin, Plavix, Xarelto, or Eliquis will be instructed to restart these medications on a day instructed by Dr. Incavo or his staff.
Pain Medications: You will be discharged from the hospital with prescription(s) for pain medication. Take the pain medication as prescribed and only for as long as you have pain. The pain medications are only to be taken as needed. For the first few days, you may likely require dosing more often (ie. Every 6 hours), but you may reduce the frequency of use as you can tolerate. You should NOT OVERUSE these medications due to side effects, which may include: nausea, itching, constipation, drowsiness as well as dependence. Prescriptions for narcotic medications will generally NOT BE written for longer than 6 weeks after your surgery and cannot be called into your pharmacy. PLEASE NOTE DUE TO DEA REGULATIONS, ALL NARCOTIC PRESCRIPTIONS WILL HAVE TO BE HANDWRITTEN ON A TRIPLICATE PRESCRIPTION AND WILL ONLY BE AVAILABLE TO BE PICKED UP IN THE OFFICE DURING NORMAL BUSINESS HOURS.
Constipation: Constipation can easily occur when patients are hospitalized, given general anesthesia and given large doses of pain medications. You should increase your fiber, fluids and bowel regulating foods to your diet prior to surgery. Good foods include prunes, prune juice, whole grain breads, oatmeal, fruits and vegetables. Fiber supplements such as Metamucil, Citrucel, or FiberCon can also be helpful. If you are unable to have a bowel movement by the third day following surgery a laxative may be necessary. There are many good over the-counter medications that you may use including: Colace, Sennakot, Phillips Milk of Magnesia, Miralax, Dulcolax. If you are still unable to achieve a bowel movement with these methods, a glycerin suppository or use of an enema may be necessary.
Driving: You may return to driving 1-2 weeks after surgery once you are walking comfortably with a cane.
Dental Visits: Dental procedures should be postponed for 6 months after joint replacement surgery. When you do return to the dentist, antibiotics will need to be taken 1 hour prior to your visit to prevent infection of the joint replacement. Please inform your dentist that you have a joint replacement. Antibiotics can be prescribed by our office or by your dentist. You will take Amoxicillin 2000 mg (four 500 mg tablets) 1 hour prior to dental work. If you are allergic to penicillin, you will be given Clindamycin 900 mg (three 300 mg tablets) to be taken 1 hour prior to procedure. If a dental visit is necessary or urgent before 6 months after joint replacement, please contact our office.
If you have any additional questions please contact our office at 713-441-3569 or via MyChart.

Standing Hip Abduction
Stand holding on to a solid object for support and balance.
Raise your heels off the floor standing on the balls of your feet.
Work to hold this position for 30 seconds.

Standing Hip Flexion
Stand holding on to a solid object for support and balance.
Raise your heels off the floor standing on the balls of your feet.
Work to hold this position for 30 seconds.

Standing Heel Raises
Stand holding on to a solid object for support and balance.
Raise your heels off the floor standing on the balls of your feet.
Work to hold this position for 30 seconds.
Work on the above exercises for 5-10 minutes at a time at least two times daily.
You will need to have the FREE Adobe Acrobat Reader installed on your system to view this document. Download the Reader by clicking on the Acrobat icon below